Assessa
About Progressive multifocal leukoencephalopathy (PML)
Progressive multifocal leukoencephalopathy (PML) is a rare infection caused by the John Cunningham virus (JC virus). The JC virus is present, but latent, in the majority of the population [Honce, Nagae & Nyberg, 2015]. Its activity is usually suppressed by the body’s immune system. In individuals with a compromised immune system, the virus may become re-activated, causing cell loss and destroying myelin-producing oligodendrocytes, resulting in severe demyelination and inflammation known as PML. Multiple sclerosis patients receiving immunosuppressant treatment have an increased risk of developing PML [Honce, Nagae & Nyberg, 2015].
Detection and diagnosis of PML
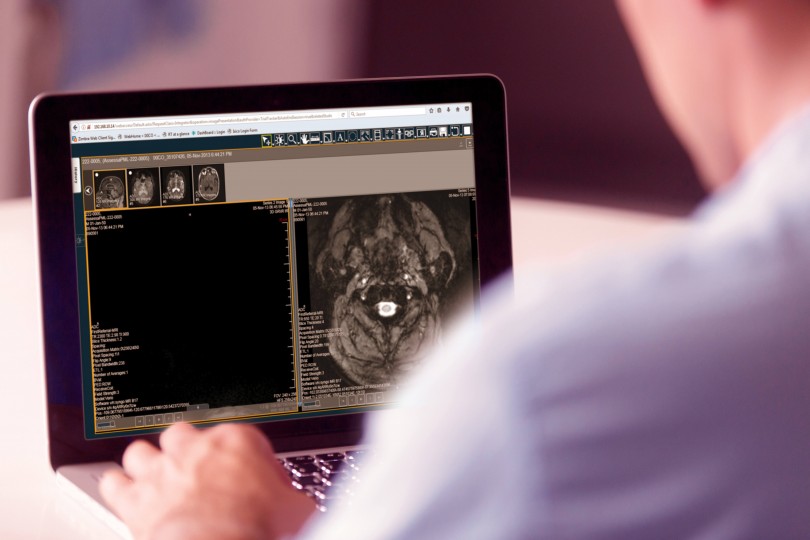
MRI is a sensitive test to detect PML in asymptomatic cases [Wattjes et al, 2014]. Furthermore, as clinical manifestations of PML can be subtle, diagnosis can be delayed from days to months. In these cases, MRI may be a useful tool to offer patients, however interpretation requires specialist neuroradiology expertise. To diagnose PML, physicians should take into account the following factors: patients’ clinical symptoms, MRI findings, and CSF analysis. For final diagnosis CSF–PCR for JCV DNA should be used [Baldwin and Hogg, 2013].
Though PML can be fatal, close monitoring of high-risk individuals enables physicians to work with patients and the care team to make the best, informed treatment decisions.
Case Study - Assessa PML
Assessa PML is an online digital platform that supports the early and/or asymptomatic detection of progressive multifocal leukoencephalopathy (PML). IXICO has developed the Assessa PML platform in collaboration with Pharma and leading clinical/academic experts.
Assessa provides neurologists with access to neuroradiology experts specialized in the differential diagnosis of suspect PML lesions from Magnetic Resonance Imaging (MRI).
Assessa PML in the clinic
- provides access to expert neuroradiologists for a standardized radiological read
- securely captures and transfers clinical data and MR images from referring neurologists to expert neuroradiologists
- stores pseudo-anonymized data and MR images securely, compliant with international data protection regulations
- returns actionable information to the referring neurologist to inform treatment decisions
- supports the longitudinal monitoring and MRI follow-up of suspect cases
- enhances medical care and knowledge exchange, including facilitating discussion of difficult cases among expert neuroradiologists